Surgery is often the main treatment for earlier-stage colon cancers. The type of surgery used depends on the stage (extent) of the cancer, where it is, and the goal of the surgery.
Some early colon cancers (stage 0 and some early stage I tumors) or polyps can be removed during a colonoscopy, where a long flexible tube with a small video camera on the end is inserted through the person's rectum and into the colon. When done this way, the doctor does not have to cut into the abdomen.
• For a polypectomy, the cancer is removed as part of the polyp, which is cut at its stalk (the area that resembles the stem of a mushroom). This is usually done by passing a wire loop through the colonoscope to cut the polyp from the wall of the colon with an electric current.
• A local excision is a slightly more extensive procedure that can be used to remove superficial cancers and a small amount of nearby tissue from the wall of colon.
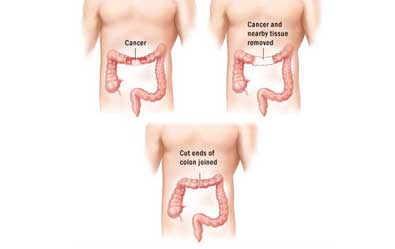
A colectomy is surgery to remove all or part of the colon. Nearby lymph nodes are removed as well.
• If only part of the colon is removed, it is called a hemicolectomy, partial colectomy, or segmental resection. The surgeon removes the part of the colon with the cancer and a small segment of normal colon on either side of the cancer. Usually, about one-fourth to one-third of your colon is removed, but this depends on the size and location of the cancer. The remaining sections of your colon are then reattached. Nearby lymph nodes are removed at this time as well. Typically, at least 12 are removed.
• If the entire colon is removed, it is called a total colectomy. Total colectomy is not often needed to treat colon cancer. It is generally used only if there is disease in the part of the colon without the cancer, such as hundreds of polyps (in someone with familial adenomatous polyposis) or, sometimes, inflammatory bowel disease.
A colectomy can be done in 2 ways:
• Open Colectomy: The surgery is done through a single long incision (cut) in the abdomen.
• Laparoscopic-assisted colectomy: The surgery uses several smaller incisions and a laparoscope, a thin lighted tube with a small video camera on the end that lets the surgeon see inside the abdomen. Special long instruments are inserted through the other incisions to remove part of the colon and lymph nodes.
Because the incisions are smaller in a laparoscopic-assisted colectomy than in an open colectomy, patients often recover faster and may be able to leave the hospital sooner than they would after an open colectomy. But this type of surgery requires special expertise, and it might not be the best approach for everyone. If you are considering this type of surgery, be sure to look for a skilled surgeon who has done many of these operations.
Overall survival rates and the chance of the cancer returning are thought to be similar between an open colectomy and a laparoscopic-assisted colectomy.
Any type of colectomy is major surgery, so it's important for you to be as healthy as possible if you are having it. If the tumor is large and has blocked your colon, the doctor may use a colonoscope to put a stent (a hollow metal or plastic tube) inside the colon to keep it open and relieve the blockage for a short time to help prepare for surgery a few days later.
If a stent can't be placed for a blocked colon or if the tumor has caused a hole in the colon, surgery may be needed right away. This usually is the same type of colectomy that's done to remove the cancer, but instead of reconnecting the segments of the colon, the top end of the colon is attached to an opening (stoma) in the skin of the abdomen to allow stool to come out. This is known as a colostomy and is usually temporary. Sometimes the end of the small intestine (the ileum) instead of the colon is connected to a stoma in the skin. This is called an ileostomy. Either way, a removable collecting bag is attached to the stoma to hold the waste.
Once you are healthier, another operation (known as a colostomy reversal or ileostomy reversal) can be done to attach the ends of the colon back together or to attach the ileum to the colon. Rarely, if a tumor can't be removed or a stent placed, the colostomy or ileostomy may need to be permanent.
Some patients have colon cancers that have spread but also have tumors blocking the colon. For patients with this problem, sometimes surgery is done to relieve the blockage without removing the part of the colon containing the cancer. Instead, the colon is cut above the tumor and attached to a stoma (an opening in the skin of the abdomen) to allow stool out. This is known as a diverting colostomy. It can often help the patient recover enough to start other treatments (such as chemotherapy).
If the cancer has spread to only one or a few spots in the lungs or liver (and nowhere else), surgery may be used to remove it. This is generally done only if the cancer in the colon or rectum is being removed as well (or was already removed). Depending on the extent of the disease, this might help you live longer, or it could even cure you. Deciding if surgery is an effective option to remove areas of cancer spread depends on their size, number, and location.
Possible risks and side effects of surgery depend on several factors, including the extent of the operation and your general health before surgery. Problems during or shortly after the operation can include bleeding from the surgery, infections at the surgery site, and blood clots in the legs.
When you wake up after surgery, you will have some pain and probably will need pain medicines for a few days. For the first couple of days, you may not be able to eat or you may be allowed limited liquids, as the colon needs some time to recover. Most patients are able to eat solid food again in a few days.
Rarely, the new connections between the ends of the intestine may not hold together completely and may leak, which can lead to infection and might require further surgery. It's also possible that the incision in the abdomen might open up, becoming an open wound.
After the surgery, you might develop scar tissue in your abdomen that can cause organs or tissues to stick together. These are called adhesions. Sometimes, adhesions can block the bowel, requiring further surgery.
Colostomy or ileostomy: Some people need a temporary or permanent colostomy (or ileostomy) after surgery. This can take some time to get used to and might require some lifestyle adjustments. If you have a colostomy or ileostomy, you will need help learning how to manage it. Specially trained ostomy nurses or enterostomal therapists can do this. They will usually see you in the hospital before your operation to discuss the ostomy and to mark a site for the opening. After the operation they may come to your house or an outpatient setting to give you more training.
© Dr. Parvinder S. Lubana. All rights reserved. | Developed & Design by ipromptsolution.com